OCD
SPECIFICATION: The biological approach to explaining and treating OCD: genetic and neural explanations; drug therapy
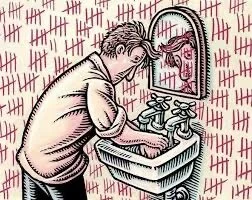
THE EMOTIONAL CHARACTERISTICS OF OCD
Extreme anxiety and distress. Being aware of OCD tendencies may create embarrassment or shame. Disgust may be apparent in people with obsessions with hygiene or germs.
THE BEHAVIOURAL CHARACTERISTICS OF OCD
Obsessive behaviours are repetitive and observable, e.g. hand washing or repeatedly checking the same things. Sufferers may engage in behaviours they feel they need to do due to fear of something dreadful happening, which in turn creates further anxiety. Everyday functioning may be hindered due to anxiety. Social impairment and difficulty conducting social and interpersonal relationships may be evident.
THE COGNITIVE CHARACTERISTICS OF OCD
Reoccurring intrusive thoughts encourage acts they think will reduce anxiety, e.g. cleaning door handles and washing hands. May experience doubtful thoughts, such as the fear of overlooking something. Sufferers may realise their thoughts are irrational or inappropriate to share with others and struggle to control them consciously, causing further anxiety.
Possible exam questions for mental disorders include:
Outline the emotional characteristics of phobias/depression/OCD
Outline the behavioural characteristics of phobias/depression/OCD
Outline the cognitive characteristics of phobias/depression/OCD
GENETIC EXPLANATIONS FOR OCD
Genetic explanations suggest OCD is transmitted through specific genes, and there is a biological basis for the disorder.
To investigate this, family and twin studies have been conducted to compare the probability of OCD between them and the general population. Specific genes have also been investigated to understand their influence, and gene-mapping studies have been conducted to compare sufferers with non-sufferers.
Grootheest et al. (2005) conducted a meta-analysis of over 70 years of twin studies into OCD. Twin studies involve comparing identical twins with non-identical twins. As identical twins have the same genetics, if their probability of having OCD is significantly higher than non-identical twins, this would imply a genetic influence for the disorder supporting genetic explanations. If non-identical twins have a higher rate, then this would imply environmental factors play a strong role (psychological), which would undermine genetic explanations.
This meta-analysis concluded that OCD did appear to have a strong genetic basis, with genetic influence ranging from 45-65% within children. Genetic influences were estimated to range from 27-47% in adults. First-degree relatives have also been found to have an 11.7% chance of OCD compared to only 2.7% of the general population when compared to non-sufferers Nestadt et al. (2000).
Other genetic explanations have suggested the COMT gene, which regulates and causes higher dopamine production, may contribute to OCD as it has been more commonly found in sufferers of OCD than non-sufferers (Tukel et al. 2003). Other genetic explanations have focused on the SERT gene, which affects the transportation of serotonin and causes lower levels of this. In one case study, a mutation of this gene was found in two unrelated families where six of the seven members had OCD (Ozaki et al. 2003).
RESEARCH EVIDENCE
Summary: Genetic and Environmental Contributions to the Child Behavior Checklist Obsessive-Compulsive Scale - A Cross-cultural Twin Study
Background on OCD Studies:
The lifetime prevalence of OCD in adolescents ranges from 1.9% to 4.1%, with higher rates in girls.
Genetic and environmental influences on OCD have been studied through family and twin studies, with mixed results.
Molecular genetic studies have focused on genes related to the monoamine pathway, with varied findings.
Authors: James J. Hudziak, MD; C. E. M. van Beijsterveldt, PhD; Robert R. Althoff, MD, PhD; et al.
Published in: Arch Gen Psychiatry. 2004;61(6):608-616. doi:10.1001/archpsyc.61.6.608
Objective: To determine the genetic and environmental contributions to obsessive-compulsive behaviour in children using the Child Behavior Checklist Obsessive-Compulsive Scale (CBCL OCS) through a twin study conducted in the Netherlands and the USA.
Design:
Utilized data from the Netherlands Twin Registry (NTR) and the Missouri Twin Study (USA/MOTWIN).
Participants included twins aged 7, 10, and 12 years from NTR and mixed-age twins from MOTWIN.
Participants:
4246 twin pairs (aged 7), 2841 twin pairs (aged 10), and 1562 twin pairs (aged 12) from the NTR.
1461 mixed-age twin pairs (average age ~9 years) from the USA/MOTWIN.
Measures:
Genetic and environmental influences, sex differences, and sibling interaction/rater contrast affect CBCL OCS.
Results:
Significant additive genetic influences (45%-58%) and unique environmental influences (42%-55%) were found.
The NTR sample noted Shared environmental influences only at age 12 (16%).
Sex differences were observed in the mixed-age USA/MOTWIN sample but not in the NTR samples.
No dominance, sibling interaction, or rater-contrast effects were found.
Consistent findings across ages and cultures.
Conclusions:
Obsessive-compulsive behaviour is influenced by genetic factors (about 55%) and unique environmental factors (about 45%) in younger children.
Common environmental influences are only significant at age 12.
The influence of genetic factors on obsessive-compulsive behaviour is consistent across the sexes.
The CBCL OCS effectively identifies children with OCD, demonstrating high sensitivity and moderate specificity.
OTHER RESEARCH
The study had multiple aims:
Determine Genetic and Environmental Contributions: Assess the contributions of genetic and environmental factors to Child Behavior Checklist Obsessive-Compulsive Scale (CBCL OCS) scores.
Sex-Genetic Interactions: Investigate the presence of sex-genetic interactions.
Age Influence: Analyze the impact of age on genetic/environmental influences on CBCL OCS scores by examining twin samples aged 7, 10, and 12 years, as well as a mixed-age sample of twins aged 8 to 12 years.
Cultural Differences: Examine if genetic/environmental contributions differ between the Netherlands and the United States.
METHODS
Subjects and Procedure
Netherlands Twin Registry (NTR): Data were collected from a large ongoing twin-family study in the Netherlands involving twin pairs at ages 7, 10, and 12. After excluding pairs with missing data, the sample included 4246, 2841, and 1562 twin pairs at these respective ages.
Missouri Twin Study (USA/MOTWIN): This study involved 1461 twin pairs from a diverse ethnic background in Missouri, collected through an ongoing project. Zygosity was determined through questionnaire items validated against DNA analysis.
Measures
Child Behavior Checklist (CBCL): This is a questionnaire for parents to report 118 problem behaviours of their child over the past six months, scored on a 3-point scale (0 = not true, 1 = sometimes true, 2 = often true). The CBCL OCS, developed using factor analysis, includes 8 items indicative of OCD, with a scoring range from 0 to 16.
Data Analyses
Differences in Means: Mean scores and variances were calculated using Mx software. Differences by sex and zygosity were tested using likelihood ratio tests.
Models: Structural equation modelling was used to estimate genetic and environmental influences on CBCL OCS scores. The basic model included additive genetic factors (A), common/shared environment factors (C), and nonshared environment effects (E). The best-fitting models were determined by comparing full and reduced models using goodness-of-fit statistics and the Akaike information criterion.
RESULTS
Differences in Means
Sex Differences: Significant sex differences in CBCL OCS scores were found in all three samples, with boys scoring higher in the USA/MOTWIN sample and girls scoring higher in the Dutch samples.
Twin Correlations
Genetic and Environmental Influences: MZ twin correlations were consistently higher than DZ correlations, indicating genetic influences. Shared environmental influences were significant only in the NTR-12 sample.
Model Fitting
Best-Fitting Models: The best models for most samples included additive genetic (A) and unique environmental (E) contributions. Shared environmental (C) influences were significant only in the NTR-12 sample. No substantial sex differences were observed in the Dutch samples, while minor sex effects were noted in the USA/MOTWIN sample.
COMMENTARY
Key Findings
Heritability: CBCL OCS scores are highly heritable, with genetic influences ranging from 45% to 58% and unique environmental influences ranging from 42% to 55%.
Stability Across Age, Sex, and Culture: Genetic and environmental contributions to CBCL OCS scores are stable across different ages, sexes, and cultures, with some variation noted at age 12 and in the USA/MOTWIN sample.
Implications for OCD Screening: The high heritability and consistent findings across different groups suggest the CBCL OCS is a reliable tool for identifying children at risk for OCD. Future research should focus on self-reports from children and adolescents to improve screening sensitivity and specificity.
LIMITATIONS
Parent-Only Reports: The reliance on parent reports may underrepresent the prevalence of OCD symptoms, as parents might not fully recognize or report their child's behaviours.
Developmental Changes: Further studies are needed to track developmental changes and sex differences in OCD prevalence during adolescence.
The study highlights the significant genetic and environmental contributions to childhood obsessive-compulsive behaviour. It underscores the importance of developmentally sensitive screening approaches to identify and support children with this condition.
UNIVERSITY OF UTAH
Researchers at the University of Utah have found powerful evidence that trichotillomania, one of the most common OC spectrum disorders, could be inherited. When they created a litter of mice that lacked the gene Hoxb8, the animals began to lick and nibble at their fur until they went bald and their skin became covered in sores.
It's thought that Hoxb8 could be involved in behaviour such as hair-pulling in trichotillomania and hand-washing in OCD.
EVALUATION OF THE GENETIC THEORY OF OCD
Strong research evidence supports genetic explanations. Twin and family studies have shown higher concordance rates for OCD compared to the general population. This suggests some element of genetics is involved; however, how much is uncertain.
The fact that not all twins share OCD tendencies despite having the same genetics suggests that it cannot be genes alone that cause OCD. This biological explanation is reductionist and oversimplified. This clearly shows there are environmental stressors that must play a part in triggering OCD, which needs to be factored in, too, and genetic explanations are unable to account for this.
A diathesis-stress model may be better suited to explaining OCD as it factors in both genetics and psychological factors such as environmental stressors. This suggests some people may have a genetic vulnerability to develop OCD, providing the right environmental triggers cause its onset. This would be a more appropriate explanation as it explains why identical twins may not share the disorder. It can also successfully account for the high concordance rates between family members and provide a more holistic explanation for the development of OCD.
Research evidence suggests there is not one specific gene responsible for OCD, and many scattered genes throughout the human genome contribute in small ways towards an individual’s overall risk of developing OCD. Research by Leckman et al. (1986) found OCD was one form of expression for the same genes that determine Tourettes syndrome. The obsessional behaviours seen between the two disorders are similar to what is found in autistic children as well as those suffering from anorexia nervosa. This suggests OCD is not one specific gene nor a single isolated disorder but one on a spectrum linked to other disorders. The fact that OCD appears in childhood more commonly due to genetic factors than in adulthood implies there may be different types of OCD with different causes, too.
Another weakness is family members may often display different forms of OCD behaviour;. At the same time, some adults become obsessive about constantly washing dishes; children may become obsessed with arranging dolls, for example. If the disorder were inherited, it would be assumed that the behaviour would be similar between family members, but this is not always the case. This is where psychological explanations may be better suited as the child may learn the obsessive behaviour from their parents modelling it. They may then demonstrate the same tendencies due to learning rather than genetics. This may explain the high concordance rates among family members as the behaviour may be learned from one another rather than genetic.
NEURAL EXPLANATIONS FOR OCD
Neural explanations for OCD have focused primarily on Serotonin and Dopamine levels affecting OCD behaviour.
High levels of dopamine causing OCD is one explanation, and a study by Szechtman et al. 1998 found that when animals were given drugs that increased dopamine levels, their behaviours resembled that of obsessive behaviours found in people with OCD.
In contrast, low levels of serotonin in patients have been linked to OCD.
This link is drawn on the fact that Pigott et al. (1990) found anti-depressant drugs that increase serotonin activity have been found to reduce obsessive tendencies and symptoms in patients. Other types of antidepressants which do not increase serotonin activity are ineffective, which suggests low levels of serotonin are linked to the disorder. PET scans on the brain have also found low serotonin levels in sufferers, providing more physical evidence of the involvement of this neurotransmitter.
Other neural explanations suggest that several areas within the sufferers' frontal lobe are abnormal, which may cause the disorder.
PET scans have shown OCD sufferers having high levels of activity in the orbital frontal cortex (OFC), which is associated with higher-level thought processes and converting sensory information into thoughts. The caudate nucleus located in the basal ganglia is responsible for suppressing signals from the OFC. When damaged or abnormal, it fails to suppress minor “worry” signals, alerting the thalamus, which signals the OFC, which acts as a “worry circuit”.
Comer (1998) linked serotonin and dopamine to these frontal lobe areas, believing they caused them to malfunction. This appears valid, as dopamine is the main neurotransmitter in the basal ganglia.
Evaluating Neural Explanations for OCD
Research support for neural explanations comes from a study by Pichichero (2009). Case studies from the US National Institute Of Health showed that children with throat infections often displayed sudden indications of OCD symptoms as well as Tourette’s shortly after infection. This supports neural explanations as infections can affect the neural mechanisms that may underpin OCD itself, and the two disorders are thought to occur through similar gene activations.
If neural mechanisms are abnormal, genetic factors influencing their development would cause them. Therefore, neural explanations are reductionist and oversimplified. They alone can not explain the disorder, as genetics are likely the root cause.
The research into serotonin and dopamine being linked to OCD is based on correlational research, and we cannot certainly establish cause and effect due to this. It may well be that high dopamine levels or low serotonin levels are the effects of having OCD rather than the cause itself. The fact that not all sufferers of OCD respond to serotonin-enhancing drugs adds weight to this possibility, and other causes need to be considered.
Although research seems to suggest a link with neural mechanisms, we still can not completely explain how they may cause OCD. It’s possible unknown variables may lie in between that are causing the unaccounted-for disorder.
Possible exam questions for the biological approach to explaining OCD:
Outline genetic explanations for obsessive-compulsive disorder (OCD)
Outline neural explanations for obsessive-compulsive disorder (OCD)
Outline a criticism of genetic explanations for obsessive-compulsive disorder (OCD)
Outline and evaluate the biological approach to explaining OCD (12 marks AS, 16 marks A-level). Genetic explanations suggest that OCD is inherited and that individuals inherit specific genes that cause it. Genetic explanations have focused on identifying particular genes implicated in OCD. Two genes linked to OCD are the COMT gene and the SERT gene.
The SERT gene (Reduced Serotonin Reuptake Transporter), also known as the 5-HTT gene) is linked to the neurotransmitter serotonin and affects the transport of serotonin (hence, Serotonin Transporter), causing lower serotonin levels. Sufferers have faulty serotonin receptors that reuptake the neurotransmitter too quickly. This means serotonin neurons don’t fire, and the person has a hypo serotonin system, e.g., low neurotransmitter availability. The reason why low levels of serotonin might be relevant to OCD is that low levels are associated with anxiety, fear and obsessive thoughts.
EVALUATION
Two methods are available when looking for support for the genetic model: comparing the genetic profiles of those with OCD to normal controls and/or looking at family concordance rates.
One strength of the biological explanation of OCD comes from research from family studies. Lewis (1936) examined patients with OCD and found that 37% of the patients with OCD had parents with the disorder and 21% had siblings who suffered. Research from family studies, like Lewis, provides support for a genetic explanation of OCD. However, it does not rule out other (environmental) factors playing a role as family members may learn behaviours operantly, classically or indeed via vicarious reinforcement.
The genetic model of OCD is well supported by twin studies. For example, MZ twins have an 87% concordance rate, whilst DZ twins only have a 48 % concordance rate; this suggests a strong genetic component, as identical twins share 100% of their DNA.
However, there are several things wrong with this research. Firstly, meta-analyses of twin studies and OCD have shown very varied results; some research has shown that MZ twins have a much lower concordance rate of 50%. Nestadt et al. (2010) conducted a review of previous twin studies examining OCD. They found that 68% of identical twins and 31% of non-identical twins experience OCD. Low reliability means less certainty. This may be because the research was unreliable in the past, e.g., old definitions of OCD before DSM V may have made samples unreliable.
Alternatively, MZ teens could have a higher concordance because they are the same gender (DZ twin studies rarely control for gender), and they look identical. Therefore, it is likely that they are treated as the same person rather than as separate identities, meaning that it could be some proportion of the environment that has caused this disorder. This is supported by the fact that MZ twins are never 100 % concordant for OCD, so the environment must play some at least 13-32 % risk.
Further support for this comes from trauma victims and those suffering from PSTD, wherein 30% of cases develop OCD a year after trauma, again showing the effect of the environment. However, PSTD sufferers may also have a genetic temperament that predisposes them to anxiety
Serotonin reuptake transporter (SERT) is a key regulator of serotonin neurotransmission and a major target of antidepressants. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), that block SERT function work very well for patients with OCD, suggesting that problems with low availability of serotonin may indeed be at the root of OCD.
However, this genetic and biochemistry hypothesis does not account for individual differences because the research does not explain why one individual develops OCD and another develops a different mental disorder because low serotonin levels are also found in other mental disorders. Thus, these biochemical abnormalities are not specific to OCD and may be true of any form of mental distress. SSRIs are treatments for all of these disorders btw, which begs the question of how each of these disorders can be biologically unique if the same drug works for each of them.
Psychological therapy (CBT) can be a very successful treatment, and this is difficult to account for in the serotonin hypothesis
Chicken and egg type situation
Moreover, the biochemistry hypothesis is always certain, and it came first. Do low levels of serotonin cause OCD, or does OCD cause low levels of Serotonin? Clearly, the genetic argument would say that the SERT gene came first, and it changes Serotonin, which in turn causes OCD. Still, some people get OCD after a traumatic event, and thus, their serotonin changes afterwards.
Not all who suffer from OCD have a faulty SERT gene or respond to SSRIs. This may mean that OCD is a polygenetic disorder and has different genes involved in its cause. This may explain why some sufferers develop different types of OCD, e.g., cleaning versus safety.
The COMT gene is another gene associated with the production of, which regulates the neurotransmitter dopamine. One variation of the COMT gene results in higher levels of dopamine, and this variation is more common in patients with OCD than in people without OCD. High levels of Dopamine affect thinking and movement, and this may be why sufferers have difficulties with thoughts and behaviours.
OUTLINE NEURAL EXPLANATIONS OF OCD
Neural explanations of OCD focus on neurotransmitters as well as brain structures.
Neural explanations suggest that abnormal levels of neurotransmitters, in particular serotonin and dopamine, are implicated in OCD, but these were discussed above with genetics.
Neural explanations also suggest that particular regions of the brain, in particular the basal ganglia and orbitofrontal cortex, are implicated in OCD.
Brain Structures
Neural explanations suggest that particular regions of the brain might not work efficiently. For example, the OFC has been implicated as causal in OCD because it is responsible for decision-making and organisation, which are clearly compromised in sufferers of OCD. The OFC is also responsible for primitive responses, e.g., innate responses that are hard-wired to respond to dangers, like loud noises, fire, certain creatures, and heights, e.g., the innate response to fearing attack would be to check you are safe. In OCD, this mechanism may be difficult to stop. One suggestion is that the heightened activity in the orbitofrontal cortex increases the conversion of sensory information to actions (behaviours), which results in compulsions. The increased activity also prevents patients from stopping their behaviours.
For example, after a visit to the bathroom, your primal instinct to survive by avoiding germs is brought to your attention. You may decide to wash your hands to remove any harmful germs you may have encountered.
Once you have performed the appropriate behaviour, the PFC reduces inactivation, and you stop washing your hands and go about your day. It has been suggested that if you have OCD, your PFC is over-activated. This means the obsessions and compulsions continue, leading you to wash your hands again and again.
Interestingly, one of the major Serotonin circuits runs directly through the OFC. This area may not function correctly because it does not receive the right amount of serotonin.
FMRIS supports differences in OFC of controls and OCD sufferers, e.g., the scans show higher activity. Scans are robust, reliable, and scientific, but not all OCD suffers show this abnormality, so it is not a complete explanation.
The basal ganglia
The basal ganglia are a brain structure involved in multiple processes, including movement coordination. Patients who suffer head injuries in this region often develop OCD-like symptoms following their recovery. Furthermore, Max et al. (1994) found that when the basal ganglia is disconnected from the frontal cortex during surgery, OCD-like symptoms are reduced, providing further support for the role of the basal ganglia in OCD.
OTHER Evaluation
.One weakness of the biological explanation for OCD is that it ignores other factors and is reductionist. For example, the biological approach does not consider cognitions (thinking) and learning. Some psychologists suggest that OCD may be learnt through classical conditioning and maintained through operant conditioning. Stimulus (for example, dirt) is associated with anxiety, and this association is then maintained through operant conditioning, where a person avoids dirt and continually washes their hands. This hand washing reduces their anxiety and negatively reinforces their compulsions.
Is OCD an extreme form of Mere cat syndrome?
The evolutionary hypothesis of OCD. Humans with a psychological horror of germs survived the evolutionary competition with less germ-phobic ancestors. OCD may represent the end of an adaptive trait that protected our clans from diseases potentially far worse than COVID-19, for example! Or imagine if we lived in dangerous environments where crime, muggings and murder were common; a hyper-vigilant relative might save your life! Maybe OCD is adaptive for some members of the clan. Or maybe it represents a safety mechanism that is faulty and too stimulated.
Genes alone do not determine who will develop OCD—they only create vulnerability. Thus, they are not a direct cause as other factors must trigger the disorder. The Stress diathesis model can explain these differences, e.g. the gene predisposes you to OCD but must have a stressor to activate it (e.g., traumatic event, head injury, drugs, poor childhood)
ECLECTIC APPROAH? NATURE AND NURTURE?
Biological Treatments for OCD: Drug Therapy
Biological therapies for OCD
For biological therapies for obsessive-compulsive disorder, the AQA A-level psychology specification states you need to know only about drug therapies. Which drugs are used to treat OCD? Antidepressants are the most commonly used treatment for both OCD and depression.
OCD SPECTRUM DISORDERS
More than a compulsion
As the science behind obsessive-compulsive disorder (OCD) is unravelled, it is becoming clear that many other illnesses may share its underlying cause. Scientists call this family of related illnesses obsessive-compulsive (OC) spectrum disorders.
Numerous people suffer from an OC spectrum disorder
The relationship of these disorders to OCD is supported by the fact that they all feature intrusive impulses (similar to obsessions in OCD) followed by uncontrollable actions (similar to OCD compulsions).OCD SPECTRUM DISORDERS
More than a compulsion
As the science behind obsessive-compulsive disorder (OCD) is unravelled, it is becoming clear that many other illnesses may share its underlying cause. Scientists call this family of related illnesses obsessive-compulsive (OC) spectrum disorders.
Numerous people suffer from an OC spectrum disorder
The relationship of these disorders to OCD is supported by the fact that they all feature intrusive impulses (similar to obsessions in OCD) followed by uncontrollable actions (similar to OCD compulsions).
Major OC spectrum disorders
Trichotillomania - a failure to resist the urge to pull out hair, resulting in noticeable hair loss
Body dysmorphic disorder (BDD) - sufferers imagine they have a defect in their physical appearance, for example, a pock-marked complexion or a weak chin. They frequently check themselves in the mirror or try to camouflage their body parts.
Kleptomania - a failure to resist impulses to steal objects not needed for personal use or financial gain
Compulsive sexual behaviour - uncontrollable sexual thoughts or behaviour that makes the sufferer distressed or causes them to have personal, job or criminal problems
Compulsive shopping - excessive and unnecessary shopping that leads to personal, job or financial problems
Pathological gambling - A loss of control over gambling habits that results in heavy financial losses and personal or legal problems
Intermittent Explosive Disorder - violent outbursts of rage that can result in serious assaults and destruction of property
Pyromania - an uncontrollable urge to start fires, associated with a release of tension
Controversial theories
Some researchers think that eating disorders such as anorexia nervosa and bulimia are also OC spectrum disorders. But this theory is highly controversial and bitterly disputed.
However, they undeniably share many features. The excessive fear of gaining weight in anorexia nervosa resembles an obsession, and relentless dieting is often described as difficult to resist and distressing, just like an OCD compulsion.
Another candidate for inclusion as an OC spectrum disorder is hypochondriasis. This is a fear of having a serious illness based on a person's misinterpretation of symptoms of disease in their own body
DRUG THERAPY
Antidepressants are the most commonly used biological therapy for treating OCD as well as depression.
Low serotonin levels are believed to play a role in influencing OCD with the orbital frontal cortex (also known as the worry circuit) malfunctioning.
Using antidepressants is believed to bring levels back to normal but also help reduce anxiety, which is associated with OCD.
The preferred drugs are SSRIs (selective serotonin reuptake inhibitors), with adults commonly prescribed Fluoxetine (Prozac).
Children aged six years are prescribed Sertraline, while those aged eight or over are prescribed Fluvoxamine.
The treatment lasts 12 to 16 weeks. SSRIs work by inhibiting serotonin reuptake, which is released into the synapses from neurons by blocking receptor cells. This increases serotonin levels and stimulation at the synapses, alleviating OCD tendencies.
Tricyclics are also used exclusively for OCD and block the transportation mechanism, which reabsorbs serotonin and noradrenaline into the pre-synaptic cell after firing. As serotonin builds up in the synapse, this prolongs their activity and eases transmission of the next impulse.
Anti-psychotic drugs have also been used, which aid in lowering dopamine levels, as high levels have also been associated with the disorder. These are normally given if SSRIs do not prove effective due to their side effects.
Drugs such as Benzodiazepines lower anxiety levels by slowing down activity in the central nervous system by enhancing GABA activity (gamma-aminobutyric acid). GABA dampens many neurons within the brain by locking on to GABA receptors. This opens a flow of chloride ions into the neuron, which reduces the effects of other neurotransmitters and reduces activity in the central nervous system, relaxing the individual.
Drug therapy evaluation
Research evidence shows drug therapies are effective compared to placebo in the treatment of OCD. Pigott et al. (1999) reviewed studies testing the effectiveness of drug therapies and concluded that SSRIs had been consistently proven to be effective in reducing OCD symptoms.
Tricyclic drugs have also been found to be more effective than SSRIs; however, they carry more serious side effects, which may make them inappropriate as the initial drug to use. SSRIs may be more appropriate as a first option, and if they are not effective, then Tricyclic trials may be considered appropriate.
Drug therapies do not cure OCD, which may make them inappropriate as they may mask the symptoms of a biological disorder rather than cure it. Also, CBT is effective in treating OCD for some patients, and this treatment carries no risk of side effects, unlike drug therapies. Therefore, CBT may be more appropriate to try first rather than drug therapies.
Drug therapies such as SSRIs carry side effects such as heightened levels of suicidal thinking, loss of sexual appetite, irritability, sleep disturbance, headaches and loss of appetite. Depending on the patients themselves, they may not always be appropriate, especially if sufferers of OCD have a history of depression or children who may struggle to cope.
Antidepressant drugs are cheap to manufacture, easy to administer and user-friendly when compared to psychological treatments such as CBT, which can be time-consuming.
They are fast-acting and effective, allowing individuals to manage their symptoms and lead normal lives. For these convenience reasons alone, they may be more appropriate for many patients who cannot spare the time to try other, more time-consuming options.
Possible exam questions for the biological therapies for OCD:
Outline how drug therapies are used to treat obsessive-compulsive disorder (OCD)
Outline and evaluate biological therapies for obsessive-compulsive disorder (OCD). Re-uptake inhibitors: SSRIs, SRIS etc (too little Serotonin)
Old class of drugs: tricyclics (too little Serotonin)
Other psychotropic drugs:
Anxiety: Benzodiazepines (too little GABA)
Anti-psychotics: relate to COMPT gene (too much Dopamine (antagonist)
KEYWORDS
OCD
OCD symptoms as applied to drug efficacy
SERT gene
COMPT gene
Agonist (e.g., stimulants that increase the availability of a neurotransmitter)
Antagonist (e.g., blockers that decrease the availability of a neurotransmitter)
Anti-depressants
re-uptake inhibitors
Selective Serotonin reuptake inhibitors (SSRIs) Prozac and Citalopram
Serotonin reuptake inhibitor (SRIS)
Serotonin and norepinephrine (NORADRENALIN) reuptake inhibitors (SNRIs) SRIS
Other anti-depressants: Tricyclic anti-depressants (TCAs): Clomipramine (Anafranil)
Anxiolytic drugs (anti-anxiety drugs) Benzodiazepines: Valium, Diazepam, Lorazepam, Xanax
Alternative treatments (psychological) Cognitive behavioural therapy (CBT) Exposure and Response Prevention (ERP) – which is a CBT therapy specific to OCD
(then check back after you have finished writing the essay to see if you have not missed key ideas and terminology)
AQA Mark scheme for A01
Attempt to increase or decrease levels of neurotransmitters or the activity of neurotransmitters in the brain.
The purpose is to decrease anxiety, lower arousal, and lower blood pressure or heart rate.
Antidepressants – SSRIs – prevent the reuptake of serotonin and prolong its activity in the synapse to reduce anxiety / normalise the ‘worry circuit.’
Tricyclics – block the transporter mechanism that re-absorbs both serotonin and noradrenaline, again prolonging their activity
Anti-anxiety drugs – such as benzodiazepines – enhance the activity of GABA and, therefore, slow down the CNS, causing relaxation
SNRIs – more recent drugs which also increase levels of serotonin and nor-adrenaline and are tolerated by those for whom SSRIs are not effective.
OUTLINE DRUG TREATMENTS
One of the biological explanations for OCD suggests that the disorder is the result of low levels of serotonin in the brain. This is because research shows that many sufferers are thought to have an irregular SERT gene, which causes serotonin to be re-absorbed too quickly before it can affect the brain and behaviour. As Low levels of serotonin cause low mood, anxiety and obsessive thought, which are the most prominent symptoms experienced by patients with OCD, it is hypothesised that stopping this re-uptake mechanism of serotonin will also stop OCD symptoms from occurring. As a result of this logic, reuptake inhibitors, a class of anti-depressants, such as SSRIs, SRIS, and SNRIs, are the primary first-line treatment for OCD.
SSRIs (selective serotonin reuptake inhibitors) are the most popular type of reuptake inhibitors given in this group; these include drugs like Prozac and Citalopram. SSRIs work by blocking the process in which Serotonin is reabsorbed back into the axon terminal vesicles after they are released, so instead of getting reabsorbed, the neurotransmitter stays -- at least temporarily -- in the gap between the nerves, called the synapse. The logic is that if you keep levels of Serotonin in these neural circuits higher, communication between the serotonin neurons is strengthened, and thus, mood, thought, and anxiety are regulated.
EVALUATION POINTS
Effectiveness of SSRIs E.g., write a paragraph that shows research support. Ensure it is PEELED
Then, critique the SSRI research. There are several critique points:
SSRIs don’t work for all people with OCD; this may be because not all people with OCD have the SERT gene
SSRIs can make some people worse
With alternative drug treatment (tricyclic), side effects are worse if this doesn’t work, anti-psychotic COMPT gene)
SSRIs have horrible side effects which may have very adverse effects on a person’s life, for example, sexual dysfunction and emotional strait-jacketing
Because OCD occurs in youth, it is not uncommon to give them to adolescents and, in some cases, children.
Side effects common to all
Age-related OCD side effects, e.g., medication under 25
Vulnerable, negative-plasticity, brain hard-wires behaviours under 25 but especially when teens
MESSES WITH MIND suicide and homicide ideation
Symptoms, not cause /Aspirin analogy (statistics that OCD often begins after a traumatic episode)
If Americans do not have insurance, it is cheaper than CBT (NHS full, long waiting list).
It is easier to do (especially as OCD might fear treatment and not go or might be less able to access CBT, distance, etc.)
SSRIs don’t work straight away for six weeks, so during that time, they make people feel worse - OCD feel worse for six weeks, so the Clinician prescribe Benzo temporarily, which works on GABA.
Alternative treatments psychological
If you want to check that you have included all the relevant A03, check your textbook, a fellow student, Exampro, or even online sites like Simply Psychology.
AQA mark scheme A03:
Possible limitations:
Side effects
Patient as a passive recipient of treatment
Dependency
Comparison with alternative treatments
Credit other relevant limitations.
NOW ORDER this A03 so that it flows logically and has a coherent structure
BTW, I am not going to order it for you, but you can read my version below to see the order I have put the A03 in
EVALUATION
SSRS as a treatment for OCD is supported by randomised drug trials, which compare the effectiveness of SSRIs to placebos. These trials compare the effectiveness of SSRIs and placebos (a ‘drug’ with no pharmacological value).
Soomro et al. (2008) reviewed the research examining the effectiveness of SSRIs. They found that SSRIs were more effective than placebos in the treatment of OCD in 17 different trials. This supports the use of biological treatments, especially SSRIs, for OCD.
However, the success of SSRIs in research has been questioned, as pharmaceutical companies have been accused of designing studies that make SSRIs look good. More importantly, many of the people who fund the studies on SSRIs, by and large, have a vested interest in seeing them approved, e.g., links to pharmaceutical companies, the DSM, and the APA.
Moreover, the mechanism of approval is also misunderstood. People think it's safe and good for them if the FDA approves an SSRI. The FDA isn't saying that the benefits outweigh the harms; they are just saying they are marginally better than placebo at a particular point in treatment (usually the first few months).
Most drug trials don't measure long-term exposure, only short-term effects of treatment, so if you take Xanax as an example, it looks like a very successful treatment if researched in its first four weeks! However, it doesn't show any efficacy after about four weeks and patients on it over one month show an opposing pattern of behaviour by becoming increasingly anxious, what is commonly referred to as “Down-Regulation” and in the case of Xanax; this would be the “Down-Regulation” of GABA receptors. In short, there seems to be a lack of concrete research for assessing what happens to people on OCD drugs for long amounts of time.
In any case, the use of SSRIs as a treatment is not effective for all sufferers. For example, only 30% of patients make a significant improvement, and 20% make some improvement, whilst 30% do not improve at all. In addition, some people with OCD find that SSRlS can exacerbate their condition further. This may be because not all who have OCD have a problem with the SERT gene.
In cases where patients seem resistant to Re-uptake inhibitors including the newer SNRIs) which works on noradrenalin in addition to Serotonin. They can be offered alternative drug treatments such as anti-psychotics, which reduce Dopamine activity in the brain and might fit better with the COMPT gene hypothesis of too much Dopamine as a cause. However, antipsychotics have some horrendous side effects, such as massive weight gain/diabetes and Tardive Dyskinesia and are rarely continued because of this.
Clinicians usually only prescribe tricyclic antidepressants (TCAs) after other drugs have failed to relieve OCD.TCAs are an older type of antidepressant. Only TCAs that potently inhibit presynaptic reuptake of serotonin appear to be effective in treating obsessive-compulsive disorder. Clomipramine (Anafranil) is the only tricyclic antidepressant (TCA) with this quality. They're no longer usually recommended as the first treatment for OCD because they can be more dangerous if an overdose is taken. They also cause more unpleasant side effects than SSRIs and SNRIs.
Moreover, although SSRIs might be effective in varying degrees for 50% of sufferers, the side effects of the drugs can be as problematic as the condition. Some patients experience mild side effects like indigestion, while others might experience more serious side effects like hallucinations, erection problems/sexual dysfunction, emotional straitjacketing, sleep issues and raised blood pressure. Consequently, these side effects diminish the effectiveness of drug treatments, as patients will often stop taking medication if they experience these side effects, as they seem to be problematic for the disorder.
More worrying is the trend of giving patients under the age of twenty-five, particularly teens and children, SSRIs as a treatment. This is because the brain is still very malleable (plastic) in these age groups, meaning that reliance on drug treatment could become hard-wired into the brain, leaving children and teenagers with life-long dependencies on anti-depressants. More importantly, such treatments have not been FDA-approved for children, and research has shown that an alarming number of teens suffer from suicide ideation and homicide ideation whilst taking them.
Another factor that confounds the use of treating OCD with anti-depressants is the length of time they take to work. SSRIs for example, take six weeks to show any therapeutic effect but more importantly, they make the sufferer worse before they make them better, in other words, they are known to cause extreme anxiety in the initial stages of use. This may discourage OCD patients from continuing them or even trying them. It takes an average of seven years for a person with OCD to seek help, and by this time, the condition is profoundly affecting their ability to function adequately. Thus, many people with OCD might not be able to cope with feeling worse in the interim, and this may prohibit them from accessing SSRIs as a treatment. Some clinicians may offer short-term use of benzodiazepines (BZs) to ameliorate the initial effects of the SSRIs. Benzodiazepines such as Valium and Xanax are GABA agonists, so they may help OCD with their anxiety levels whilst adjusting to SSRIs. BZs are renowned for being highly addictive and can also cause increased aggression and long-term memory impairments. As a result, BZs are usually only prescribed for short-term treatment.
Another key criticism levied at drug treatments is that a significant proportion of sufferers develop OCD after a traumatic event, so the use of drugs will not cure the problem, only the symptoms. In other words, OCD should also be treated psychologically. Furthermore, once a patient stops taking the drug, they are prone to relapse, suggesting that psychological treatments may be more effective as a long-term solution.
In addition, critics also point out that although increasing serotonin levels may have a therapeutic effect, this does not mean that lack of serotonin is a contributory cause. The “Aspirin analogy is often used to make this point, e.g., taking Aspirin may reduce the symptoms of a headache, but that does not mean that a lack of Aspirin causes headaches! Indeed, SSRIs are used to treat depression as well as OCD; this begs the question of how OCD and depression are different if the medications are the same.
Research suggests that the most effective treatment for OCD (70% success rate) is Cognitive Behaviour Therapy (CBT), in particular, a type of CBT specifically designed to help OCD sufferers called Exposure Response Prevention (ERP). Exposure Response Prevention is a therapy that encourages you to face your fears and let obsessive thoughts occur without ‘putting them right’ or ‘neutralising’ them with compulsions. If ERP is combined with medications, in some situations, patients may benefit more.
The only disadvantage of Psychological treatments like CBT is that they require a patient to be motivated. One of the strengths of drug treatments is they are non-disruptive to a person’s lifestyle and can be taken until the symptoms subside. As a result, drugs are likely to be more successful for patients who lack the motivation to complete intense psychological treatments.
Another strength of drug treatment is its cost. Biological treatments, including anti-depressants and anti-anxiety drugs, are relatively cost-effective in comparison to psychological treatments, like cognitive behavioural therapy (CBT). Consequently, many clinical establishments prefer the use of drugs over psychological treatments, as they are a cost-effective solution for treating OCD, which is beneficial for health service providers.
The above points are also relevant to a discussion on determinism and reductionism if you want to go there …